Coding for Developmental & Mental Health Screening
ICD-10 and CPT Coding for billing and tracking pediatric developmental and mental health screening
Coding and billing for screening performed in the medical home can help cover the costs of the work done and the instruments used to monitor for developmental delays, maternal depression, risky substance use, suicidality, and mental health disorders. Screening reimbursement is complicated because state and private insurers may differ on how many screens may be reimbursed during 1 visit or in 1 year. Some payers contract with participating providers to bundle developmental or mental health screening with preventive care or direct their providers to bill differently from the American Medical Association's CPT guidelines. Detailed coding and billing, even if not paid by Medicaid or the insurer, are useful to track work value (RVU).
Key Points
Importance of coding
Accurate, detailed coding, even for items not currently
reimbursable, helps reflect the actual clinical effort and identifies codes that
may need to be reimbursable in the future to optimize care for children with
special health care needs.
ICD-10 vs. CPT Codes
ICD-10 Codes
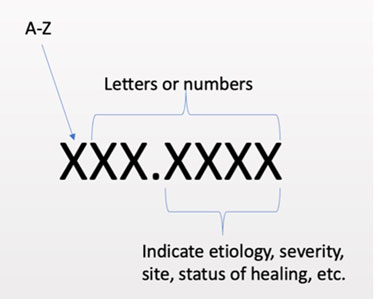
ICD codes refer to the specific condition or situation being addressed. These codes are a standard diagnostic language to communicate what you address during a visit. They are 3-7 characters long and allow for specificity.
- Each CPT code has an RVU (relative value unit) used by payers to determine payment
- Medicare uses a conversion factor for each RVU. In 2022, for example, 1 RVU was equivalent to $34.6062)
- 99213 – 5:
- 99213 = 2.66 RVUs
- 99214 = 3.75 RVUs
- 99215 = 5.29 RVUs
- Miscoded encounters can lead to significantly decreased compensation for the work provided.
ICD-10-CM Codes for Screening
ICD-10-CM codes from A00.0 through T88.9, Z00-Z99 must be used to identify diagnoses, symptoms, conditions, problems, complaints, or other reason(s) for the encounter/visit. The following ICD-10-CM Z codes are frequently used for screening.
Z00.1*- Well-child check/Encounter for newborn, infant, and child health examinations, including routine developmental screening.
- Z00.129 - well-child visits >28 days, without abnormal findings
- Z00.121 - well-child visits >28 days, with abnormal findings
- A Z00.1* health exam is always listed first as the primary reason for the visit.
Z13.3*- Encounter for screening examination for mental health and behavioral disorders.
- Z13.30 …… unspecified
- Z13.31 Encounter for screening for depression
- Z13.32 Encounter for screening for maternal depression (this can be coded in the mother’s chart but not the infant’s)
- Z13.39 Encounter for screening examination for other mental health and behavioral disorders
Z13.4*- Encounter for screening for certain developmental disorders in childhood.
- Z13.40 Encounter for screening for unspecified developmental delays
- Z13.41 Encounter for autism screening
- Z13.42 Encounter for screening for global developmental delays (milestones)
- Z13.49 Encounter for screening for other developmental delays
Z13.89 Encounter for screening for other disorder (when not listed elsewhere in the ICD-10 codes) – usually not necessary to report in addition to a well-child exam.
CPT Codes for Screening
CPT codes are used to request reimbursement for the expense of each screening instrument, including the scoring and documentation. Documentation should include the date, patient's name, name and relationship of the informant (when information is provided by someone other than the patient), name of the instrument, score, and name and credentials of the individual administering/scoring the instrument. The physician must document that they reviewed the score in the context of the patient presentation and discussed the results with the patient/family as part of the related E/M or preventive service. Associate the CPT code with an appropriate ICD-10-CM code, often the Z00.12* well-child code.
| CPT Code | Examples of Screens |
| 96110 Developmental screening (e.g., developmental milestone survey, speech and language delay screen, autism screen) | M-CHAT, ASQ-3rd Edition, PEDS, SWYC |
| 96127 Brief emotional/behavioral assessment (e.g., depression inventory, attention-deficit/hyperactivity disorder [ADHD] scale) | ASQ-SE, SCARED, Vanderbilt, PSC, PHQ-2, PHQ-9 or adolescent version, Connors |
| 96160 Administration of patient-focused health risk assessment instrument (e.g., health hazard appraisal) | CRAFFT, AUDIT, BSTAD, S2BI, DAST-20 |
| 96161* Administration of caregiver-focused health risk assessment instrument (e.g., depression inventory) for the benefit of the patient | Edinburgh Postnatal Depression Scale (English), PHQ-2, PHQ-9 administered to caregiver during a baby’s visit |
Payers vary in their requirements and reimbursements for screening instruments.
Modifiers 25 and 59
Modifier 25 appends one service with a second, separately identifiable E/M service. Modifier 25 states that the procedure performed should be considered separate from the visit. There is no need to use Modifier 25 for routine screening in a well-child visit.
Modifier 59 indicates a distinct procedural service (non-E/M service). Documentation should demonstrate the distinction between procedure(s) with each other and/or the visit to support billing both. Sometimes, a modifier 59 might be required if two of the same type of screens are used during the same visit, but this can vary by payer.
Coding Examples
The ICD-10-CM codes (reasons for the visit) are listed first, followed by associated CPT (procedure) codes and modifiers.
Example 1: Well-child Check with Routine Screening and an Ear Infection
| CPT Codes | Associated ICD-10-CM Codes |
| 99392*25 Early childhood preventive medicine services | Z00.121 Well-child check with abnormal findings (primary diagnosis) |
| 96110 x 2 developmental screens (reimbursement varies) | Z00.121 |
| 99213 distinct E/M service | H66* suppurative otitis media |
Example 2: 4-Month Well-child Check with Abnormal Maternal Depression Screen
| CPT Codes | Associated ICD-10-CM Codes^ |
| 99391*25 Infant preventive medicine services SWYC | Z00.121 Well-child check with abnormal findings (primary diagnosis) |
| 96110 Developmental screen – Child development screening | Z00.121 |
| 96161 Caregiver assessment (Edinburgh) Mother depression screening | Z00.121 |
Example 3: Routine Adolescent Health Check with New Concern for Anxiety
| CPT Codes | Associated ICD-10-CM Codes |
| 99394*25 Adolescent preventive medicine services | Z00.121 Well-child check with abnormal findings (primary diagnosis) |
| 96127x2 Brief emotional/behavioral assessment (PHQ-9 Depression) and (SCARED anxiety) | Z00.121 Z13.39 Encounter for screening examination for other mental health and behavioral disorders |
| 96160*59 Patient-focused health risk assessment instrument (CRAFFT Health Hazard/Alcohol use)^ | Z00.121 |
Example 4. Screens Reviewed During a Behavioral Health/Medication Management Follow-Up Visit
| CPT Codes | Associated ICD-10-CM Codes |
| 99215*25 Time-based E/M (includes face-to-face and non-face-to-face time) | F90.2 ADHD combined type (primary diagnosis) |
| 96127 x 3 Brief emotional/behavioral assessment | F90.2
F40.10 Social anxiety disorder |
Example 5. Developmental and Autism Screening Performed During an Unrelated Sick Visit
| CPT Codes | Associated ICD-10-CM Codes |
| 99213*25 E/M services | H66* suppurative otitis media (primary diagnosis) |
| 96110 x2 Developmental screens | Z134.42 screening for global developmental delay |
Example 6. Positive Depression Screen and Screening for Substance Use During an Unrelated Visit
| CPT Codes | Associated ICD-10-CM Codes |
| 99214 Time-based E/M services (includes face-to-face and non-face-to-face time) | R21 Rash
and other nonspecific skin eruption (primary diagnosis)
Z71.89 Other specified counseling |
| 96127 Brief emotional screener (PHQ-9/A) | Z13.30
Encounter for mental health and behavioral screening
F32.9 Major depressive disorder, single episode |
| 96160 Health risk assessment (DAST-10) | Z13.30 |
Example 7. Wart Removal Plus New Behavioral Concerns
| CPT Codes | Associated ICD-10-CM Codes |
| 17110 Destruction of benign lesions other than skin tags or cutaneous vascular lesions; up to 14 lesions | B07.9 Viral warts, unspecified (primary diagnosis) |
| 99202*25 Time-based E/M, new patient (includes face-to-face and non-face-to-face time) | Z73.9 Problem related to life management difficulty, unspecified |
Example 8. Subsequent Wart Removal Plus Discussion of Screening Results
| CPT Codes | Associated ICD-10-CM Codes |
| 99214*25 Time-based E/M (includes face-to-face and non-face-to-face time) | F90.0 ADHD, inattentive type |
| 96127 x2 Brief emotional screeners (both Vanderbilts) | F90.0
Z13.39 Encounter for screening examination for other mental health and behavioral disorders |
| 17110 Destruction of benign lesions other than skin tags or cutaneous vascular lesions; up to 14 lesions | B07.9 Viral warts, unspecified (primary diagnosis) |
Resources
Information & Support
Related content on the Portal includes:
For Professionals
Coding Fact Sheets (AAP)
Codes for medical home visits, mental health care, oral health, screening, and more that clinicians can submit to insurance
carriers for payment of medical services; American Academy of Pediatrics.
Coding for Pediatric Preventive Care, 2022 (Bright Futures) ( 2.0 MB)
2.0 MB)
Current Procedural Terminology (CPT), Healthcare Common Procedure Coding System (HCPCS) Level II, and International Classification
of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes most commonly reported by pediatricians in providing preventive
care services; American Academy of Pediatrics/Bright Futures.
Pediatric ICD-10-CM 2024, 9th Edition (AAP)
Condenses the vast ICD-10-CM code set into only pediatric-centered guidelines and codes; American Academy of Pediatrics Committee
on Coding and Nomenclature (COCN).
Pediatric Coding Basics: An Introduction to Medical Coding (AAP)
available for a cost; AAP Committee on Coding and Nomenclature (COCN)
Pediatric Evaluation and Management Coding Quick Reference Card 2024 (AAP)
All 2024 changes in evaluation and management (E/M) codes - available for purchse only; American Academy of Pediatrics and
American Committee on Coding and Nomenclature (COCN).
AAP Coding Hotline and Hassle Factor Form
Online form for help with coding; American Academy of Pediatrics.
Authors & Reviewers
| Author: | Alanna Brickley, MD |
| Reviewer: | Jason Fox, MPA/MHA |
| 2019: first version: Jennifer Goldman, MD, MRP, FAAPA; Jason Fox, MPA/MHAR; Andrea Reeder, MBA, CPCR |